Cancer begins as a single cell gone subtly, then catastrophically, wrong. That cell’s DNA—life’s instruction set—acquires changes that tip its behavior from disciplined citizen to rogue operator. Over months to decades, that rogue cell and its descendants become an ecosystem, then a province, then—sometimes—a nation that invades others. The astonishing part is that each step follows rules, rules we now know well enough to fight back.
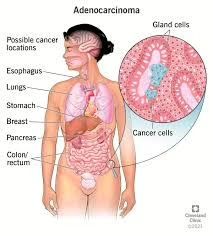
What “cancer” really is
Biologically, cancers are diseases of genes and cell behavior. Most human tumors carry “driver” DNA changes that corrupt three classes of genes: proto-oncogenes (which become growth-promoting oncogenes when mutated or overactive), tumor suppressor genes (the brakes that, when disabled, fail to stop growth or trigger death), and DNA-repair genes (the maintenance crews that prevent and fix errors). When the balance is lost, cell growth and survival become unmoored from normal tissue rules. (Cancer.gov, Cancer.org)
The canonical framework for how cancers behave is the “Hallmarks of Cancer”—properties tumors evolve to thrive: sustaining proliferative signaling, evading growth suppressors, resisting cell death, enabling replicative immortality, inducing angiogenesis (new blood vessels), activating invasion and metastasis, reprogramming cellular energetics, avoiding immune destruction, and more. This conceptual map has been refined across two decades to include new “dimensions,” like phenotypic plasticity and non-mutational epigenetic reprogramming. (RSC Education, PubMed)
Where cancer comes from: mutations, chance, and exposure
The origins of the first malignant cell

Mutations accrue from exogenous insults—like tobacco smoke, ultraviolet light, alcohol, asbestos, infectious agents (HPV, HBV, H. pylori), and ionizing radiation—and endogenous processes—like DNA replication errors, oxidative stress, and age-related changes. The International Agency for Research on Cancer (IARC) maintains definitive classifications of carcinogens and the cancer sites they cause; cigarette smoke and solar UV are group-1 carcinogens with sufficient evidence in humans. (monographs.iarc.who.int)
Inherited predispositions can “pre-load” the path: in Lynch syndrome, mismatched DNA repair raises lifetime risk of colorectal, endometrial, and other cancers; careful tumor testing for microsatellite instability and immunohistochemistry now routinely flags who should get germline testing and tailored surveillance. (CDC, NCBI, Cancer.gov)
As mutations accumulate, evolution does the rest. Pioneering work in 1976 proposed that tumors are clonal evolutions: diverse subpopulations compete, and selection favors the fittest clones under the pressures of the microenvironment and therapy. Modern multi-region sequencing (notably in the TRACERx project in lung cancer) directly observes this branching evolution in patients and links intratumor heterogeneity to worse outcomes. (foxchase.org, PubMed, Nature)
The deep logic of cancer genomes
Across tumor types, recurrent themes appear. Oncogenes like RAS (first flagged in the early 1980s) drive growth; tumor suppressors like RB1 (two-hit hypothesis) and TP53 (the “guardian of the genome”) are often knocked out. A panoramic survey of cancer genomes shows characteristic “landscapes”: a handful of targetable drivers amid a sea of passengers, copy-number chaos, and epigenetic alterations. (BioMed Central, Nature, PMC)
How many mutations—and which ones—matter?
Not all mutations are equal. Some are merely signatures of the processes that created them (UV makes C→T changes in a telltale pattern; tobacco does its own). Others are the steering wheel: KRAS in pancreatic and lung cancers, BCR-ABL in chronic myeloid leukemia (CML), HER2 amplification in some breast cancers. Recognizing these drivers has rewritten treatment. (ScienceDirect, ASCO, ESMO)
How tumors grow: more than runaway division
Building a malignant ecosystem
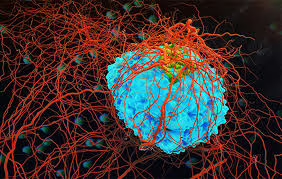
A tumor is not just malignant cells; it’s an engineered organ. It recruits blood vessels (angiogenesis)—classically articulated by Judah Folkman—so interior cells don’t starve. It co-opts fibroblasts, immune cells, and extracellular matrix to make a microenvironment that feeds growth and blunts attack. (PubMed)
Some cells within the tumor behave like cancer stem cells—rare, therapy-resistant subpopulations with self-renewal and the capacity to regenerate the tumor after treatment. While the details are debated and vary by cancer type, the therapeutic implications are profound: eradicating the bulk without touching these seeds risks relapse. Recent reviews synthesize the evidence and evolving markers. (PMC, Nature)
Evasion and plasticity
To survive in a hostile body, cancer cells disable checkpoints (p53, Rb), resist apoptosis, alter metabolism, and evade immunity. Many epithelial tumors adopt epithelial-mesenchymal plasticity—a sliding scale of state changes (often mislabeled as a simple on/off “EMT”)—that aids migration, invasion, and drug resistance. The modern view is nuanced: plasticity, not a single EMT program, underlies metastatic adaptability. (PubMed, Annual Reviews, Nature)
How cancer spreads: metastasis, the “seed and soil”
Most cancer deaths result from metastasis, not the primary tumor. In 1889, Stephen Paget’s “seed and soil” hypothesis suggested that circulating tumor cells (seeds) flourish only in compatible organs (soil). Today we map the steps: local invasion, intravasation into vessels, survival in circulation, extravasation, and colonization—each with distinct molecular demands. Modern reviews trace the molecular choreography and tumor–microenvironment dialogs. (PMC, PubMed)
How cancer kills
Cancer ends lives through several converging mechanisms:
- Organ failure: Liver, lung, or brain failure from bulky or infiltrative disease.
- Metastatic complications: Bone fractures, spinal cord compression, malignant effusions.
- Thrombosis and embolism: Hypercoagulability leads to lethal clots.
- Infection and immunosuppression: From marrow infiltration or therapy.
- Cancer cachexia: A systemic metabolic syndrome of involuntary weight and muscle loss driven by inflammatory and tumor-derived signals; it weakens patients, reduces therapy tolerance, and independently predicts mortality.
A 2024 roadmap in Nature Medicine synthesizes these paths to death and calls for trials targeting them directly—cachexia, thromboinflammation, organ-specific failure—alongside tumor control. (The Lancet)
The human toll, by the numbers
Globally, cancer remains a leading cause of death. The IARC/WHO GLOBOCAN program tallies incidence and mortality regularly; the 2021 CA Cancer Journal for Clinicians report (based on 2020 estimates) is a standard reference for burden by site and region. In the U.S., the American Cancer Society (ACS) reports steady declines in cancer mortality since the early 1990s, driven by reduced smoking, screening, and better treatments—but warns of rising incidence in some younger cohorts and worrisome trends in specific cancers. (PMC, Health)
The war (and wisdom) through time: milestones in research and care
Early clues and the birth of prevention
- 1775: Percivall Pott links soot exposure in chimney sweeps to scrotal cancer—the first strong environmental carcinogen inference and a triumph of observation. (Galleri® Test)
- 1911: Peyton Rous shows a transmissible factor (later known as a virus) can cause sarcoma in chickens—opening the door to tumor virology and, a century later, vaccines against oncogenic viruses. (humantumoratlas.org)
- 1973 onward: Bruce Ames’ bacterial mutagenicity assay becomes a workhorse to flag DNA-damaging chemicals. (BioMed Central)
The molecular era: genes and targets
- Two-hit hypothesis (Knudson) explains how RB1 loss drives retinoblastoma and inspires the general concept of tumor suppressors. TP53 emerges as an almost ubiquitous casualty across human cancers. (PMC)
- Proto-oncogenes become a thing—RAS and friends; Bishop and Varmus receive the 1989 Nobel for retroviral oncogene insights. (BioMed Central)
- Philadelphia chromosome (BCR-ABL) is nailed as the driver of CML—proof that a single fusion can fuel an entire leukemia. Imatinib arrives in 2001 and turns CML from lethal to manageable for many. (annualreport2024.aacr.org, ASCO)
- HER2 amplification in breast cancer enables trastuzumab and later agents, radically improving outcomes in that subtype. (ESMO)
The immune awakening
For a century, the idea that the immune system can control cancer flickered. The field exploded with checkpoint blockade—antibodies to CTLA-4 and PD-1/PD-L1 that lift immune brakes and unleash anti-tumor T cells. The 2018 Nobel to James P. Allison and Tasuku Honjo recognized these breakthroughs; multiple drugs now deliver deep, durable remissions in cancers once uniformly fatal. (PMC)
Screening and vaccines
- HPV vaccination dramatically cuts cervical cancer in vaccinated cohorts (real-world data from England show striking reductions among women vaccinated at younger ages). (AACR Journals)
- Low-dose CT screening in high-risk smokers reduces lung-cancer mortality (NLST trial). (PubMed)
- HBV vaccination campaigns reduce childhood hepatocellular carcinoma in endemic regions—a public-health triumph. (The Lancet)
- H. pylori eradication lowers gastric cancer incidence in high-risk populations. (GRAIL)
Today’s arsenal: how we treat cancer now
Surgery and radiation—old, precise, indispensable
Modern surgery achieves cures in many localized cancers; radiation, more focused than ever (IMRT, stereotactic techniques), sterilizes micrometastases and controls pain.
Chemotherapy—still a pillar

Cytotoxic drugs, born from wartime nitrogen mustard observations and ushered into pediatrics by Sidney Farber, remain lifesaving, particularly in combination regimens and hematologic malignancies. (PMC)
Targeted therapy—precision where biology allows
When a tumor is “addicted” to a driver (BCR-ABL, EGFR, ALK, BRAF, HER2), drugging it can be transformational. Newer agents even tackle previously “undruggable” targets like KRAS G12C; others for G12D are advancing. Yet resistance—via new mutations, bypass pathways, and phenotypic shifts—often evolves, underscoring the need for combination strategies and next-gen drugs. (Oncodaily)
Immunotherapy—retraining the body
Checkpoint inhibitors, CAR-T cells (especially in leukemias/lymphomas), oncolytic viruses, and personalized neoantigen vaccines are expanding options. Checkpoint blockade is now frontline in several cancers; CAR-T is exploring the solid-tumor barrier; individualized mRNA vaccines are in trials. (PMC)
Radiotheranostics—seek and destroy
Targeted radioligand therapy (e.g., PSMA-directed lutetium-177 in metastatic prostate cancer) delivers radiation directly to cancer cells and improves outcomes in randomized trials. (Jto)
How we know what to do: from tissue to blood, from bulk to single cells
Pathology and genomics guide modern care. Tumors are sequenced to find actionable drivers, mutational burden, microsatellite instability, and fusions. Single-cell sequencing and spatial profiling map cell-by-cell ecosystems.
Liquid biopsy—sequencing circulating tumor DNA (ctDNA)—now detects minimal residual disease, resistance mutations, and sometimes cancer itself. Multi-cancer early detection (“MCED”) tests are under study; PATHFINDER showed feasibility (with caveats), while the UK and other trials are testing population roles. A key nuance: clonal hematopoiesis (age-related mutations in blood cells) can confound ctDNA—an active research area with methods emerging to distinguish blood-derived from tumor-derived variants. (ESMO, annualreport2024.aacr.org, PMC, AACR Journals)
Tumor evolution in real time is no longer hypothetical: TRACERx follows lung tumors from surgery through relapse, proving that intratumor heterogeneity (particularly copy-number instability) portends worse outcomes and mapping how therapy sculpts clonal architecture. (PubMed, Nature)
How many scientists are fighting this?
There is no exact headcount—the cancer enterprise spans biologists, clinicians, data scientists, engineers, public-health experts, and more across thousands of institutions. But several proxies show the scale:
- The American Association for Cancer Research (AACR) reports a global membership exceeding 60,000. (ACS Journals)
- The American Society of Clinical Oncology (ASCO) lists over 45,000 members worldwide. (ACS Journals)
- Europe’s ESMO also counts tens of thousands of members across >160 countries. (PubMed)
These are only the tip of the iceberg; add national oncology societies, pathology and radiology colleges, basic science societies, and public-health bodies, and one sees hundreds of thousands of professionals engaged. The scale of funding initiatives (below) also hints at the workforce size and momentum.
The big coordinated pushes
- The United States Cancer Moonshot aims to cut the age-adjusted cancer death rate by at least 50% over 25 years and improve the experience of people living with and surviving cancer—rallying projects across agencies and sectors. (The White House)
- The European Commission’s Europe’s Beating Cancer Plan tackles the whole pathway—prevention (including HPV/HBV vaccination), screening, treatment, and survivorship—with specific actions and funding streams. (European Commission, Public Health, European Commission)
- Cancer Grand Challenges, a joint NCI–Cancer Research UK program, funds global, interdisciplinary teams with $25M per team to attack the hardest problems (five new teams were selected in 2024, including projects on early-onset cancers and T-cell recognition). (Cancer.gov, Cancer Grand Challenges)
What tomorrow looks like: serious, science-based hope
1) Earlier and smarter detection
Expect risk-adapted screening that combines age, family history, germline variants, lifestyle, microbiome, and polygenic scores to personalize who gets what and when. MCED blood tests may complement organ-specific screening in high-risk groups if trials demonstrate a net mortality benefit without unacceptable overdiagnosis. Methodological work to weed out clonal hematopoiesis artifacts is accelerating. (annualreport2024.aacr.org, PMC, ScienceDirect)
2) Therapy that tracks evolution
We’ll sequence tumors (and ctDNA) repeatedly, treating cancer as a moving target. Adaptive trials will pre-empt resistance by combining drugs against multiple nodes (e.g., EGFR + MET, KRAS + SHP2), with dosing guided by real-time biomarkers and pharmacodynamic readouts—ideas proven in principle by TRACERx and resistance studies. (Nature)
3) Immunity, version 2.0
Beyond PD-1/CTLA-4, next-wave checkpoints (LAG-3, TIGIT), personalized neoantigen vaccines (including mRNA platforms), and engineered T-cell therapies with better homing and safety switches aim to make durable immunity more common—and extend it to “cold” tumors by remodeling the microenvironment. (PMC)
4) Conquering the microenvironment and cachexia
Trials will increasingly target cachexia pathways, thromboinflammation, and organ-specific failure—treating not only tumor cells but the lethal syndromes they precipitate. (The Lancet)
5) Radiotheranostics at scale
More ligand-radiation pairs (PSMA today; others for neuroendocrine tumors, breast, and beyond) will expand “seek and destroy” options with manageable toxicity and precision. (Jto)
6) Data and AI as accelerants
Digital pathology, multimodal models (histology + genomics + radiology), and AI-assisted trial design can compress timelines from hypothesis to impact. Large consortia (e.g., Human Tumor Atlas Network) are assembling reference maps to benchmark and simulate interventions. (ESMO)
The limits we must acknowledge
Cancer is not one enemy but many; even within a single tumor, there are multiple evolutionary lineages. That’s why “cures” often give way to resistance and why combination and sequence matter. The best gains arrive when prevention and early detection intersect with biology-driven therapy and supportive care that maintains strength, dignity, and time.
What you can do (evidence-based, right now)
- Don’t smoke; if you do, get real help quitting.
- Vaccinate against HPV and HBV where recommended.
- Screen—mammography, colon screening (colonoscopy or stool tests), Pap/HPV testing, and low-dose CT for eligible smokers—on schedule.
- Maintain a healthy weight, move your body, moderate alcohol.
These steps, at population scale, have already saved millions of life-years and will save millions more. (PubMed, AACR Journals)
Endnotes & Key Sources (selected)
(Click any citation in the text to open the source.)
- What cancer is & gene classes: National Cancer Institute; American Cancer Society. (Cancer.gov, Cancer.org)
- Hallmarks of Cancer (2000, 2011, 2022): Cell; Cancer Discovery. (RSC Education, PubMed)
- Carcinogens: IARC Monographs classifications and cancer-site lists. (monographs.iarc.who.int)
- Lynch syndrome overviews and testing pathways: CDC; GeneReviews; NCI PDQ. (CDC, NCBI, Cancer.gov)
- Clonal evolution & heterogeneity: Nowell 1976; TRACERx NEJM/Nature papers. (foxchase.org, PubMed, Nature)
- Oncogene/tumor suppressor milestones: RAS; RB1 two-hit; TP53 ubiquity; genome landscapes. (BioMed Central, PMC, Nature)
- Philadelphia chromosome & imatinib; HER2 & trastuzumab. (annualreport2024.aacr.org, ASCO, ESMO)
- Folkman angiogenesis; metastasis steps & microenvironment reviews. (PubMed)
- How cancer kills—roadmap: Nature Medicine 2024. (The Lancet)
- Global burden: CA Cancer J Clin 2021 (GLOBOCAN 2020). US trends: ACS 2024 snapshots. (PMC, Health)
- Immunotherapy history & Nobel (Allison, Honjo). (PMC)
- Prevention/screening successes: HPV (England), NLCT (NLST), HBV vaccination, H. pylori eradication. (AACR Journals, PubMed, The Lancet, GRAIL)
- Liquid biopsy, MCED trials, and CH confounding. (annualreport2024.aacr.org, PMC, AACR Journals)
- KRAS G12C approval and targeted therapies: NEJM/AA. (Oncodaily)
- PSMA radioligand therapy VISION trial (NEJM). (Jto)
- Scale of the field (memberships): AACR, ASCO, ESMO. (ACS Journals, PubMed)
- Big initiatives: Cancer Moonshot; Europe’s Beating Cancer Plan; Cancer Grand Challenges (2024 teams). (The White House, European Commission, Public Health, Cancer.gov)
