Since the dawn of humanity, the human body has battled countless afflictions. Among them, psoriasis stands as one of the most ancient, persistent, and mysterious. Despite living in an age of extraordinary scientific advances, this chronic autoimmune disease continues to evade a definitive cure. For millions around the world, psoriasis is more than just a skin condition — it is a lifelong battle marked by physical pain, emotional distress, social isolation, and unanswered questions. This article will explore the deep medical reality of psoriasis, tracing its history from ancient times to today’s cutting-edge research, shedding light on the struggle of those living with this incurable disease.

What is Psoriasis?
Psoriasis is a chronic autoimmune condition that primarily affects the skin, although its reach often extends deeper into the joints and overall immune system. It triggers the rapid overproduction of skin cells, leading to scaly, inflamed, and often painful plaques on various parts of the body, commonly the scalp, elbows, knees, and lower back.
At its core, psoriasis results from the immune system mistakenly attacking healthy skin cells. This immune dysfunction accelerates the skin’s life cycle, causing the buildup of thick patches of dry, dead skin. Unlike typical skin shedding, which happens invisibly over weeks, psoriatic skin regenerates in mere days — a destructive overdrive.
The disease is non-contagious, but its visual appearance often leads to cruel misconceptions, social stigma, and emotional pain for sufferers.

The Origins: Psoriasis Throughout Human History
Psoriasis has been part of the human story for thousands of years. Ancient Egyptian texts from around 1500 BCE described scaly skin diseases resembling psoriasis. Hippocrates (460–377 BCE), often regarded as the father of medicine, referenced similar skin conditions, though at the time it was often confused with leprosy, resulting in unjust societal exile and fear.
During the Roman era, skin diseases were poorly understood, leading to the legal and religious isolation of sufferers. In medieval Europe, people with psoriasis were often labeled “unclean” — a label that had devastating consequences for their social and emotional lives.
For centuries, psoriasis was a disease without a name, lost among other misunderstood skin ailments. It was not until 1808 that the British dermatologist Robert Willan formally classified psoriasis as a distinct disease. Yet, despite its recognition, effective treatment remained elusive.

Medical Understanding and Modern Diagnosis
Modern medicine has made tremendous strides in understanding psoriasis. Today, dermatologists recognize it as a multifactorial autoimmune disorder involving genetic predisposition and environmental triggers.
Diagnosis is primarily clinical — meaning that doctors visually assess the skin’s appearance and ask about symptoms. In rare cases, a skin biopsy may be performed to distinguish psoriasis from similar conditions such as eczema.
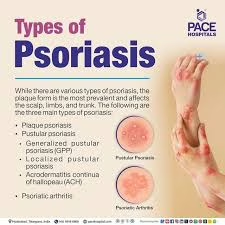
The five major types of psoriasis include:
- Plaque Psoriasis (Psoriasis Vulgaris): The most common form, featuring raised, red patches covered with silvery scales.
- Guttate Psoriasis: Small, dot-like lesions, often triggered by infections like strep throat.
- Inverse Psoriasis: Bright red, shiny lesions found in body folds.
- Pustular Psoriasis: White pustules surrounded by red skin.
- Erythrodermic Psoriasis: A severe, life-threatening form involving widespread redness, shedding, and pain.
Each type presents differently, and the disease’s severity can range from minor irritation to disabling full-body involvement.

Psoriatic Arthritis: The Pain Beyond the Skin
For around 30% of people with psoriasis, the disease progresses to psoriatic arthritis (PsA) — a condition marked by painful, swollen joints and progressive joint damage.
Symptoms include:
- Joint stiffness (especially in the morning)
- Swollen fingers and toes
- Pain in the tendons and ligaments
- Nail pitting and separation
- Fatigue
PsA can be easily misdiagnosed as rheumatoid arthritis or gout. Without proper treatment, it can lead to permanent joint damage and disability.
Psoriatic arthritis often worsens emotional distress, as patients must contend with both skin disease and joint deterioration. It is a dual burden — visible and invisible at once.
The Pain, The Struggles, and Emotional Toll
Living with psoriasis is far more than managing a skin condition. It is a relentless battle against physical pain, emotional upheaval, and societal misunderstanding.
Physical Pain
- Constant itching, burning, and cracking of the skin.
- Bleeding from even minor movements or contact.
- Sleep disruption from discomfort.
Emotional Struggles
- Depression and Anxiety: Studies show psoriasis patients are at high risk for mood disorders.
- Social Isolation: Fear of being judged or stared at often drives sufferers to withdraw.
- Employment Discrimination: Visible plaques can affect job interviews, workplace relationships, and promotions.
Patients often report feeling “trapped in their own skin,” a poignant phrase capturing the relentless and inescapable nature of the disease.
Treatments: A Constant Battle, Not a Cure
Despite decades of research, there is no cure for psoriasis. Treatments aim to control symptoms, reduce flare-ups, and improve quality of life.

Topical Treatments
- Corticosteroids: Reduce inflammation but risk thinning skin with long-term use.
- Vitamin D Analogues: Slow skin growth (e.g., calcipotriol).
- Coal Tar: Old but effective, reducing scaling and itchiness.
Systemic Treatments
- Methotrexate: A chemotherapy agent that suppresses immune overactivity.
- Cyclosporine: An immunosuppressant drug, often reserved for severe cases.
- Acitretin: An oral retinoid used primarily for pustular psoriasis.
Biologic Drugs
Biologics represent a breakthrough by targeting specific parts of the immune system. Examples include:
- Adalimumab (Humira)
- Etanercept (Enbrel)
- Secukinumab (Cosentyx)
- Ixekizumab (Taltz)
- Risankizumab (Skyrizi)
Biologics can be life-changing but are expensive, require long-term injections or infusions, and carry risks of serious infections.
Phototherapy
Controlled exposure to ultraviolet light (UVB) can slow skin cell turnover and improve lesions. However, repeated treatments can increase skin cancer risks.
Lifestyle Management
- Diet: Anti-inflammatory foods and maintaining a healthy weight can reduce flare-ups.
- Stress Management: Psychological stress is a well-known trigger.
- Smoking and Alcohol: Both are linked to worsening psoriasis.
Despite a broad arsenal, treatments often require constant adjustment, and many patients experience “treatment fatigue” from chasing fleeting periods of relief.
Scientific Research: A Mystery Still Unsolved
Modern research has uncovered much about how psoriasis works, but not why it occurs in some individuals and not others.
What We Know
- Genetics: At least 25 genetic loci have been linked to psoriasis. The HLA-Cw6 gene is the strongest association, especially with early-onset disease.
- Immune System Malfunction: T-cells wrongly attack healthy skin, triggering inflammation and hyperproliferation.
- Environmental Triggers: Infections (especially streptococcal), skin trauma (Koebner phenomenon), certain medications (e.g., beta-blockers), and stress can initiate or worsen psoriasis.
The Unanswered Questions
- Why does the immune system malfunction?
- Why do some treatments work for certain individuals and not for others?
- Why do some people develop psoriatic arthritis while others do not?
The puzzle remains stubbornly incomplete.
Experts’ Opinions
Leading dermatologists and immunologists consistently emphasize two points:
- Psoriasis is not “just a skin disease.” It is a systemic, autoimmune condition with profound physical and psychological effects.
- A cure is likely decades away, but new treatments are bringing remarkable improvements in managing symptoms.
Dr. April Armstrong, a professor of dermatology at USC, states:
“Psoriasis is a disease of the entire body, and treating just the skin is like putting a bandage over a bullet wound.”
Dr. Joel Gelfand, a prominent researcher at the University of Pennsylvania, explains:
“Biologic therapies have changed the landscape, but cost, access, and individualized response remain major hurdles.”
The consensus among experts is cautious optimism, paired with a sobering recognition of psoriasis’s complexity.

Future Directions: Hopes and Ongoing Trials
Several promising areas of research offer hope for future breakthroughs:
- New Biologic Agents: Targeting more specific immune pathways with fewer side effects.
- Small Molecule Inhibitors: Oral treatments like deucravacitinib (a TYK2 inhibitor) offer easier administration.
- Gene Therapy: Though still in infancy, altering immune responses at a genetic level could offer true remission.
- Personalized Medicine: AI and genetic profiling may soon allow doctors to tailor treatments to each individual’s unique biology.
Meanwhile, global collaborations among researchers, including the International Psoriasis Council (IPC) and National Psoriasis Foundation (NPF), aim to accelerate breakthroughs.

Conclusion
Psoriasis is as old as humanity itself, an ancient and mysterious companion in the long journey of human life.
It is a disease not only of the skin but of the soul — inflicting wounds both visible and invisible.
For those who live with it, each day is an act of courage.
Each flare-up, each stare, each moment of physical pain is met with resilience forged in silence.
Though no cure yet exists, science marches forward. Treatments are better, understanding is deeper, and hope is alive.
In the face of incurable diseases like psoriasis, empathy, support, and relentless scientific pursuit remain humanity’s greatest weapons.
The mystery persists — but so too does the strength of those who endure it.

