Introduction
Tetanus is a preventable but life-threatening disease caused by Clostridium tetani, an anaerobic, spore-forming bacterium. Despite being well understood and entirely preventable through vaccination, tetanus continues to claim lives, especially in resource-limited regions. The disease is marked by painful muscle spasms, rigidity, and potentially lethal autonomic dysfunction.
This article provides a comprehensive exploration of tetanus, integrating scientific, clinical, and epidemiological knowledge with case studies and research evidence to highlight both its historical burden and modern challenges.
1. Historical Background
1.1 Early Descriptions
- Ancient physicians described conditions consistent with tetanus. In Hippocrates’ writings, descriptions of patients with rigidity and spasms likely reflect tetanus.
- Case Example (Ancient Rome): Roman soldiers with deep puncture wounds often died within days, likely from tetanus, centuries before germ theory explained the cause.
1.2 Vaccine Development and Military Cases
- During World War I, tetanus was a major threat. Soldiers with soil-contaminated wounds often died; mortality exceeded 50% without treatment.
- By World War II, widespread tetanus toxoid vaccination nearly eliminated tetanus among wounded soldiers — a striking example of vaccine success.
2. Microbiology of Clostridium tetani
- Gram-positive, spore-forming bacillus.
- Spores resemble a “drumstick” under microscopy.
- The main virulence factor is tetanospasmin, a potent neurotoxin.
Case in Laboratory Isolation: In 1889, Kitasato Shibasaburō isolated C. tetani in pure culture from a human fatality. He demonstrated that animals injected with the culture developed identical symptoms, confirming the causative link.

3. Epidemiology
3.1 Global Burden
- High-income countries rarely see tetanus due to widespread immunization.
- In Nigeria (2015), a retrospective hospital review reported a 42% fatality rate among 122 tetanus patients, with neonatal tetanus the most lethal.
3.2 Neonatal Tetanus
- Case Example: Uttar Pradesh, India — A newborn delivered at home with unsterile scissors developed neonatal tetanus at 6 days of life, presenting with inability to suck and spasms. The infant died within 72 hours.
- Bangladesh Study (2025): Mothers lacking tetanus vaccination during pregnancy had a 36% higher risk of neonatal death compared to those immunized (PubMed).
- Hospital series in Bangladesh (2022): 10 neonatal tetanus cases were admitted; none of the mothers had received vaccination, and mortality reached 30% (bdjournals.org).
3.3 Developed Nations Cases
- United States (2019): An unvaccinated 6-year-old boy sustained a forehead laceration. Despite wound cleaning, he developed generalized tetanus, required 57 days in ICU, and generated nearly $800,000 in hospital costs. His parents declined further vaccination even after recovery.
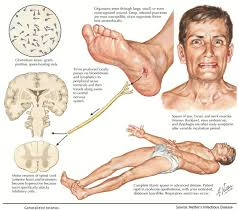
4. Pathophysiology
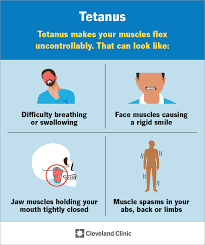
- Tetanospasmin blocks release of inhibitory neurotransmitters GABA and glycine, leading to uncontrolled motor neuron activity.
- This causes muscle rigidity, spasms, and autonomic instability.
Experimental Case: Injection of tetanospasmin into the sciatic nerve of rabbits produced localized rigidity, then generalized spasms, mirroring human disease progression.
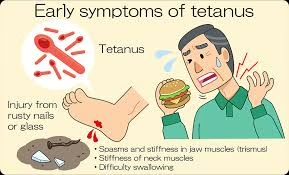
5. Clinical Features
5.1 Generalized Tetanus
- Case: Brazil (2007): A 45-year-old farmer developed lockjaw after stepping on a rusty nail. He progressed to opisthotonos and fatal spasms within 12 days, despite ICU care.
5.2 Local Tetanus
- Japan Case: A 70-year-old man presented with persistent spasm of his right arm after a hand injury. He survived with antitoxin and supportive therapy, without progression to generalized disease.
5.3 Cephalic Tetanus
- Child with Otitis Media: Presented with facial nerve palsy and trismus. Local cranial nerve involvement evolved into generalized tetanus in 48 hours.
5.4 Neonatal Tetanus
- Ethiopia: A 5-day-old infant, born at home, developed spasms and inability to suck. The mother had not received antenatal tetanus immunization. The infant died despite hospital treatment.
6. Diagnosis
- Tetanus is primarily clinical.
- Laboratory confirmation is unreliable: cultures are positive in fewer than 30% of cases (Study, Nigeria).
- Electromyography (Germany Case): Showed continuous motor unit activity even at rest, confirming diagnosis.
7. Treatment and Management
7.1 Principles
- Halt toxin production (antibiotics, wound care).
- Neutralize circulating toxin (immunoglobulin).
- Control spasms (benzodiazepines, magnesium).
- Supportive care (ventilation, nutrition).
7.2 Antibiotic Therapy
- BMJ Clinical Trial (1985): Metronidazole was superior to penicillin, lowering mortality (7% vs 24%) and reducing hospital stays (PubMed; PMC).
7.3 Immunoglobulin
- HTIG (3000–6000 IU IM) is standard; equine antitoxin used if unavailable.
7.4 Spasm Control
- Case Example: Thailand: A 35-year-old patient survived after diazepam, magnesium sulfate, mechanical ventilation, and HTIG therapy.
7.5 Autonomic Dysfunction
- Beta-blockers, clonidine, or magnesium sulfate help stabilize cardiac and blood pressure fluctuations.
8. Prevention
8.1 Vaccination
- Given as DTaP, Td, or Tdap.
- Boosters every 10 years.
Case Example (US): A vaccinated adult with a contaminated wound did not develop tetanus, highlighting protective efficacy.
8.2 Maternal Immunization
- Bangladesh (1978 study): Two maternal tetanus toxoid doses reduced neonatal mortality by 70% between days 4–14 of life (WHO/EMRO report).
9. Prognosis
- Mortality: 10–70% depending on age, ICU access, and vaccination history.
- Vietnam War: Intensive care reduced soldier mortality from >60% to <20%.
- Ethiopia Case Series: Neonatal tetanus mortality remained >80% where no ventilators were available.
10. Global Health and Elimination Efforts

- The WHO Maternal and Neonatal Tetanus Elimination (MNTE) program has eliminated tetanus in most countries.
- Uganda (2015): After targeted maternal immunization, neonatal tetanus incidence dropped dramatically, leading to elimination status.
- Conflict settings (Afghanistan 2021): Neonatal tetanus persists where health systems collapse (IJID study).
11. Research and Future Directions
- Development of monoclonal antibodies to replace HTIG.
- Trials of longer-lasting toxoid vaccines to reduce booster requirements (GAVI initiatives).
Conclusion
Tetanus is both ancient and fully preventable, yet it continues to cause avoidable deaths in unvaccinated populations. Real-world cases show how devastating it is when prevention fails, while studies and vaccination programs demonstrate the life-saving impact of immunization. With sustained public health commitment, tetanus can be eliminated as a global health problem.
References
- Ahmadsyah I, Salim A. Treatment of tetanus: procaine penicillin vs metronidazole. BMJ. 1985. PubMed, PMC
- Naha et al. Maternal tetanus toxoid immunization and neonatal mortality in Bangladesh. 2025. PubMed
- WHO/EMRO. Prevention of neonatal tetanus in Bangladesh (1978 program). WHO PDF
- IJID. Global tetanus epidemiology 1990–2019. IJID Online
- Bangladesh neonatal tetanus hospital series. bdjournals.org
- PLoS One. Decline in neonatal tetanus deaths 2000–2018. PLoS
